WHAT IS SICKLE CELL DISEASE
Understand what it is and how SCD victims suffer .
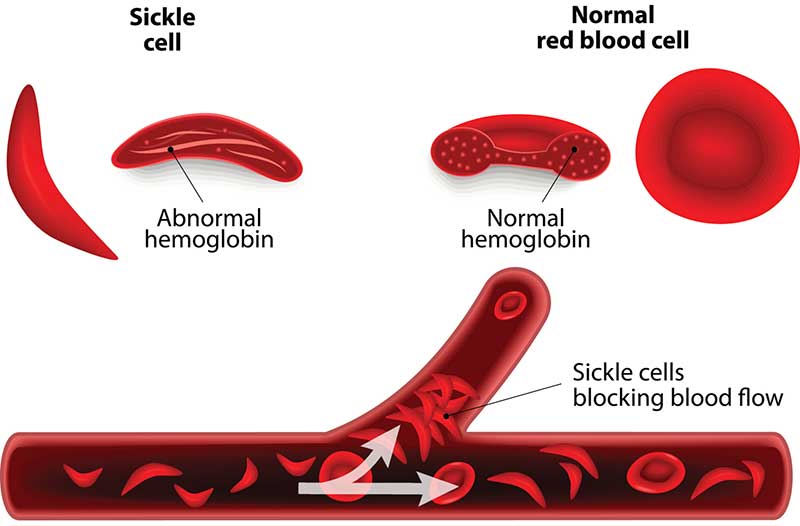
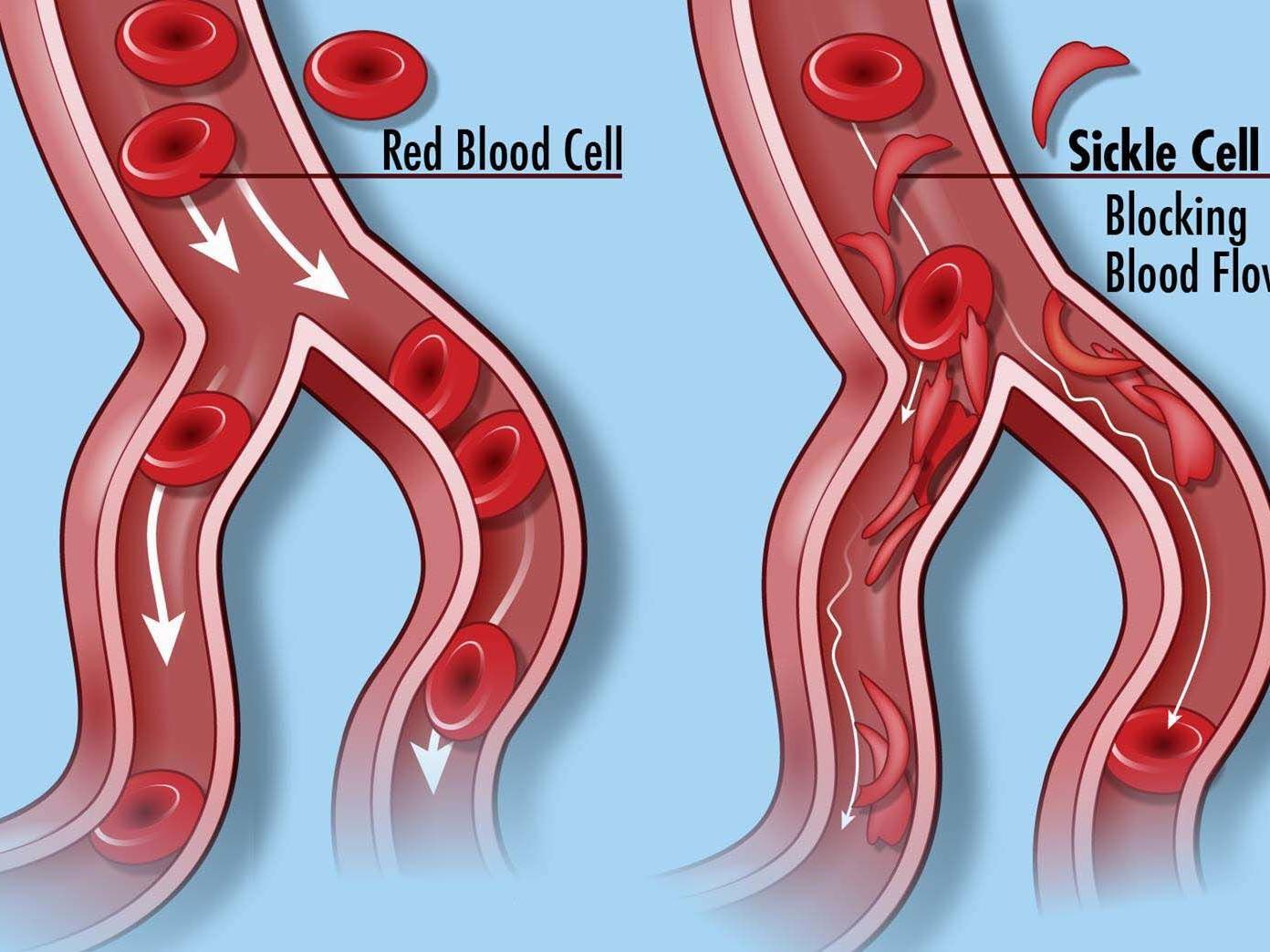
Sickle Cell Disease (SCD) is the most common monogenic blood disorder worldwide. It is associated with progressive organ damage coupled with episodes of acute illness. The episodes of acute illness result from the sticky and stiff red blood cells which clog tiny blood vessels. This often results into various conditions ranging from organ and tissue damage, anemia, increased risk of infection and painful episodes.
Worldwide, Sickle Cell Disease contributes a significant burden that is not amply addressed. It is estimated that 312,000 children is born worldwide with SCD annually. With the greatest burden existing in Sub-Saharan Africa, where 75% of the world sickle cell disease occurs.
In Africa, Uganda has the 5th highest burden, a situation aggravated by limited and inaccessible formal social support structures to aid patients and families cope better with the psychosocial burden of the disease. In addition, this has been coupled with stigmatization and discrimination of people living with sickle cell disease causing isolation from family and society.
In Uganda, it’s estimated that over 20,000 babies are born with sickle cell disease every year and 80 percent of this children die before their fifth birthday. The situation is more worrying in Northern Region where people are recovering from over 30 years of war from the Lord’s Resistance Army (LRA) which has tremendously affected livelihood in all aspects.
Problem Statement
Worldwide, the burden of Sickle Cell disease (SCD) has not been amply addressed. In Africa, Uganda has the 5th highest burden, a situation aggravated by limited and inaccessible formal social support structures to aid patients and families cope better with the psychosocial burden of the disease. In addition, this has been coupled with stigmatization and discrimination of people living with sickle cell disease causing isolation from family and society.
Over 20,000 children born in Uganda each year presents with the genetic defect. The sickle cell disease is not curable, however, if it is detected early, the symptoms can be reduced and without treatment, children die before the age of 5 years. People with sickle cell disease often suffer from many complications, such as anemia, life-threatening bacterial infections, severe physical pain, strokes and general organ failure. The disease significantly affects sufferer’s education, work and psychosocial development.
Northern Uganda has the highest prevalence of Sickle cell trait and malaria in the country standing at 18.6% and (63%) respectively according to the Sickle cell survey done in 2014 by the Ministry of Health (MoH) and Makerere College of Health Sciences. Every year about 12,000 to 16,000 children below five years die of sickle cell disease with districts of Lira, Kitgum, Dokolo, Oyam, Tororo, Jinja and Kampala witnessing a high burden with a prevalence of 20% and a disease burden ranging between 1% to 5% (Mildmay Uganda 2018 report).
However, the Sickle cell care and management in Uganda is complicated due to the complex interaction of SCD patients with the socio-ecological system. The dilemma of the persons living with sickle cell disease goes beyond grappling with the overwhelming health effects of the disease. The children living with sickle cell disease are often stigmatized, discriminated isolated and rejected in families and communities. This often forces families to hide their sick from social gatherings, church, school and community.
TREATMENT
Bone marrow transplant, also known as stem cell transplant, offers the only potential cure for sickle cell anemia. It’s usually reserved for people younger than age 16 because the risks increase for people older than 16. Finding a donor is difficult, and the procedure has serious risks associated with it, including death.
As a result, treatment for sickle cell anemia is usually aimed at avoiding crises, relieving symptoms and preventing complications. Babies and children age 2 and younger with sickle cell anemia should make frequent visits to a doctor. Children older than 2 and adults with sickle cell anemia should see a doctor at least once a year, according to the Centers for Disease Control and Prevention.
Treatments might include medications to reduce pain and prevent complications, and blood transfusions, as well as a bone marrow transplant.
MEDICATIONS
Medications used to treat sickle cell anemia include:
- Antibiotics. Children with sickle cell anemia may begin taking the antibiotic penicillin when they’re about 2 months old and continue taking it until they’re at least 5 years old. Doing so helps prevent infections, such as pneumonia, which can be life-threatening to an infant or child with sickle cell anemia.As an adult, if you’ve had your spleen removed or had pneumonia, you might need to take penicillin throughout your life.
- Pain-relieving medications. To relieve pain during a sickle cell crisis, your doctor might prescribe pain medications.
- Hydroxyurea (Droxia, Hydrea). When taken daily, hydroxyurea reduces the frequency of painful crises and might reduce the need for blood transfusions and hospitalizations. Hydroxyurea seems to work by stimulating production of fetal hemoglobin — a type of hemoglobin found in newborns that helps prevent the formation of sickle cells.Hydroxyurea increases your risk of infections, and there is some concern that long-term use of this drug might cause problems later in life for people who take it for many years. More study is needed.Your doctor can help you determine if this drug might be beneficial for you or your child. Don’t take the drug if you’re pregnant.
Get involved , show your interest to help